ILD Community Network: Linking APPs with ILD Experts



Our Alliance

Mission of the ILD Community Network
To unite, empower, and support individuals and organizations in advancing awareness, research, and care for those impacted by Interstitial Lung Disease.

Connect to ILD experts in your region
Partner with trusted ILD experts in your region to unlock your potential and achieve your goals.
ILD EXPERTS


Naomi Amudala
CRNP, MSN
Naomi Amudala, CRNP, MSN, is a highly experienced nurse practitioner specializing in rheumatology at Penn Medicine in Philadelphia, Pennsylvania. After graduating from MGH Institute of Health Professions in 2009 with a Master’s in Nursing, Naomi joined the division of Rheumatology at Boston University. Her primary focus was evaluating and managing patients with vasculitis as well as acting as co-investigator in multiple clinical trials in vasculitis. In 2018 she moved to Philadelphia and started working at Penn Medicine Rheumatology. The majority of her time continues to be dedicated to the clinical care of patients with vasculitis and other rare diseases as well as engaging in research. In 2022 Naomi joined the board of directors for RhAPP, which is a national organization for APPs and pharmacists in Rheumatology.


Christine Anderson
NP-C
Christine Anderson, NP-C, is a nurse practitioner specializing in pulmonology at Duke Health in Durham, North Carolina. She is originally from Canada and graduated from The University of Western Ontario with a Bachelors in Science in Nursing in London, Ontario back in 1999. After graduation, she moved to Durham, NC to start a nursing career at Duke University Health System. The majority of her nursing career has been in cardiology from Cardiac Step-Down to Cardiac Intensive Care Unit to the Cardiac Cath Lab. In 2005, Christine obtained a Masters in Science in Nursing with a Leadership focus and became the nurse manager of the Electrophysiology Lab at Duke Hospital. After downsizing the department, she moved over to the Duke Clinical Research Institute as a nurse clinician working on cardiology clinical trials. She truly missed patient care and went back to school and graduated with a post-master’s certificate as an Adult-Gerontologic Nurse Practitioner in 2015. Christine worked at Duke Cardiology of Lumberton for one year before coming back to main campus of Duke University Hospital and starting a new career in pulmonary medicine. Now she is the nurse practitioner for the Duke Interstitial Lung Disease Clinic where she still practices. For her last hurrah, Christine went back to school for a Doctorate of Nursing Practice degree that was awarded in 2019. Her graduate project was “Using a Smart Phrase to Improve Documentation of Supportive Care Measures in Patients with IPF”. This paper was published in the Journal for Nurse Practitioners and was presented at conferences such as the Pulmonary Fibrosis Foundation and Chest. Christine loves working with ILD patients and have learned so much over the past 9 years working in our clinic. She have been speaking about IPF and progressive ILD for past several years and have so much fun sharing my knowledge with Advanced Care Providers and providers alike.


Lisa Asfahani
PA-C
Lisa Asfahani DHSc, PA-C is a certified and state licensed Physician Assistant practicing in Rheumatology at Southland Arthritis in Temecula, California. Lisa graduated from California State Polytechnic University with a Bachelor’s degree in Biology, her Master’s degree in Physician Assistant Sciences from Loma Linda University in 2011 and her Doctorate degree in Health Sciences from A.T. Still University of Health Sciences in 2022. Lisa is experienced in both Rheumatology as well as in General Medicine and involved in numerous clinical studies in the field of Rheumatology. She is a member of several professional societies including the Association of Rheumatology Professionals (ARP), California Academy of Physician Assistants (CAPA), and RhAPP. Lisa’s goal in patient care is to treat each patient/provider interaction as an opportunity serve, to teach, and to heal. She enjoys traveling and spending time with family whenever she can.


Heather Bachert
NP
Heather D. Bachert, NP, is a board-certified Adult Nurse Practitioner and specializes in interstitial lung disease (ILD) and pulmonary fibrosis (PF) at Henry Ford Hospital in Detroit, Michigan. She earned her advanced practice training at Wayne State University and the University of Saskatchewan and is certified by the American Nurses Credentialing Center. In addition to her clinical role, Heather leads patient support groups for individuals living with ILD and PF, providing education, guidance, and a sense of community. Known for her compassionate and thorough approach, she is highly regarded by patients for her ability to explain complex conditions clearly and provide attentive follow-up care. She is currently accepting new patients and also offers telehealth services.


Shannon Benesh
DNP, NP-C
Shannon Benesh, DNP, RN-BC, AGNP-C, is a Nurse Practitioner specializing in Interstitial Lung Disease at Columbia University Irving Medical Center within the Division of Pulmonary and Critical Care. She earned her BSN from James Madison University and her MSN from Adelphi University, later completing her Doctor of Nursing Practice at Stony Brook University with a project focused on early advance care planning in ILD. Shannon has clinical experience as an RN at leading academic hospitals across various specialties and is certified as a Progressive Care Certified Nurse and Adult-Gerontology Nurse Practitioner. She is an active member of AANP, has contributed to published ILD research, and participates in national advisory boards dedicated to improving ILD care. She lives in Brooklyn with her husband and their dog and enjoys traveling, reading, running, and the occasional cocktail.


Kelley Brant
NP
Kelley Brant, NP, is a nurse practitioner specializing in pulmonology at Intermountain Health in Salt Lake City, Utah. With over 17 years of diverse clinical experience, Kelley Brant is a dedicated healthcare professional with a passion for advancing pulmonary care. A graduate of San Diego State University with a BSN, Kelley began her career as a registered nurse in high-acuity settings, including the emergency room, ICU, and urgent care, where she honed her ability to excel in fast-paced, multidisciplinary environments. Kelley earned her MSN from the University of South Alabama and is double board-certified as a Family Nurse Practitioner and Emergency Nurse Practitioner. For the past 2.5 years, Kelley has served as a nurse practitioner specializing in pulmonary medicine, with a particular focus in interstitial lung disease (ILD). As an ILD program coordinator, Kelley has gained experience in managing complex patient populations and remains actively involved in general pulmonary care, including COPD, asthma, and other respiratory conditions. Kelley also has a strong interest in research, supporting her facility’s participation in several randomized controlled trials to advance evidence-based practice. Beyond clinical work, Kelley is committed to fostering connections within the healthcare community. As a member of AANP, CHEST, and Utah Nurse Practitioners, she emphasizes professional development and collaboration to improve patient outcomes and advance the field of pulmonary care.


Michele Cera
MSN, FNP-BC


April Conlon
NP-C


Kelsey Cramer
MSN, AGACNP-BC, DNP
Kelsey Cramer, MSN, AGACNP-BC, DNP, is a board-certified adult-gerontology acute care nurse practitioner specializing in pulmonary medicine at Froedtert & the Medical College of Wisconsin. She focuses on interstitial lung disease (ILD), pulmonary hypertension (PH), and sarcoidosis. Kelsey earned her MSN and DNP from Rush University and is dedicated to delivering patient-centered care, education, and support for those managing complex lung conditions.


Kristy Delaney
APRN
Kristy Delaney, APRN, is a pulmonary nurse practitioner specializing in interstitial lung disease at The University of Kansas Health System. She has over 21 years of experience in medicine, beginning her career as a bedside RN in the Medical ICU before becoming an APRN. For the past 9 years, she has focused her practice on ILD. In addition to her clinical expertise, Kristy holds a degree in Education and is passionate about empowering patients, caregivers, and fellow healthcare professionals through education and support in the management of ILD.


Rebekah Edwards
DNP, FNP-C
Rebekah Edwards, DNP, FNP-C, is a nurse practitioner specializing in pulmonology at Norton Thoracic Institute, St. Joseph’s Hospital and Medical Center in Phoenix, Arizona. She received her Bachelor of Science in Nursing from Arizona State University and is experienced in pulmonology, cardiology, and thoracic surgery. She also received her Doctorate of Nursing Practice from Arizona State University and has practiced in pulmonology ever since.


Mary Elliot
PA-C, PhD


Kathryn Fenwick
CRNP, DNP


Heather Finlayson
PA-C
Heather Finlayson, MS, PA-C, is a certified Physician Assistant specializing in rheumatology for Summit Rheumatology in Littleton, Colorado. She previously worked at National Jewish Health Rheumatology and started at Colorado Arthritis Associates in Rheumatology in 2012. She has also taught rheumatology courses at Rocky Vista University PA program since 2022. Heather is a member of the Association of Rheumatology Professionals (ARP) (division of American College of Rheumatology-ACR), and the Association of Women in Rheumatology (AWIR). She is currently the AWIR Denver Local Chapter Co-Lead, a Rheumatology Advanced Practice Providers (RhAPP) faculty member and has served on several ACR/ARP committees.


Cori Fratelli
MSN, FNP-C
Cori Fratelli, MSN, FNP-C, is a nurse practitioner specializing in pulmonology at National Jewish Health in Denver, Colorado. She has a unique background in both basic science and clinical research, which has informed her interest in clinical medicine. Her past basic science research includes asthma, airway hyperresponsiveness, cystic fibrosis, and lung cancer. Her past clinical research includes COPD and interstitial lung disease (ILD). Presently, she is interested in how research translates into personalized medicine. Her clinical focus is mainly on ILD, but she also sees general pulmonary medicine patients, as needed.


Kyle George
PA-C
Kyle George, PA-C, is a physician assistant with over 16 years of experience in rheumatology at Saint Luke's Medical Center in Boise, Idaho. He specializes in managing autoimmune diseases such as rheumatoid arthritis and osteoporosis. Kyle collaborates with a multidisciplinary team, providing personalized and comprehensive care to his patients.


Shannon Ghizzoni
PA-C
Shannon Ghizzoni, PA-C, is a board-certified Physician Assistant specializing in rheumatology at the Columbus Arthritis Center in Columbus, Ohio. With a passion for providing comprehensive care to patients with rheumatic conditions, Shannon focuses on patient education, disease management, and improving quality of life. She is dedicated to staying current with the latest advancements in rheumatology and fostering collaborative relationships with patients and healthcare teams to deliver personalized, evidence-based care.


Audrey Gibson
PA-C, MsPAS
Audrey Gibson, MSPAS, PA-C is a board-certified rheumatology physician assistant at the Arthritis Center of North Georgia in Gainesville, Georgia. She holds dual bachelor’s degrees in biology and psychology from Lipscomb University and earned her Master of Science in Physician Assistant Studies from South University in Savannah, Georgia. Audrey is a certified densitometrist with a clinical focus on rheumatoid arthritis, psoriatic arthritis, lupus, spondyloarthropathies, inflammatory myopathies, and osteoporosis. She is an active member of the Society of Physician Assistants in Rheumatology, the Georgia Society of Rheumatology, the American College of Rheumatology, and the American Academy of Physician Assistants. Audrey also serves as a faculty advisor for the Rheumatology Advanced Practice Providers (RhAPP).


Jessica Glennie
MSN, APRN
Jessica Glennie, MSN, APRN, is a certified nurse practitioner, specializing in pulmonology, who has worked in outpatient pulmonary medicine at the Cleveland Clinic in Cleveland, Ohio for 8 years. She manages patients in the interstitial lung disease program, including care of patients with idiopathic pulmonary fibrosis, autoimmune related interstitial lung disease, hypersensitivity pneumonitis, occupational lung diseases, and drug-induced interstitial lung disease. She is co-director of the Cleveland Clinic’s ILD multidisciplinary conference.


Jeanette Hart
PA-C
Jeannette Hart, PA-C, is a board-certified physician assistant with over 13 years of experience specializing in rheumatology at Kadlec Clinic Rheumatology in Richland, Washington. She earned her Master of Clinical Health Services (MCHS) through the University of Washington’s MEDEX Physician Assistant Program in 2012. She began her career in private practice and successfully navigated transitions through both a hospital acquisition and a merger with a large healthcare system—all while refining her clinical expertise and leading efforts to improve patient access, operational efficiency, and best practices in rheumatology care. Committed to advancing healthcare delivery, Jeannette pursued a second master’s degree in Health Administration (MHA), further strengthening her leadership in clinical operations. She is now co-founder and co-owner of PNW Arthritis and Rheumatology, a private rheumatology practice opening October 1, 2025. Jeannette is passionate about education and mentorship, regularly precepting PA students and family medicine residents in her community. She is also the Pacific Northwest Director for RhAPP (Rheumatology Advanced Practice Providers) and has proudly served on its faculty since its inception.
ILD Community Network Educational Events
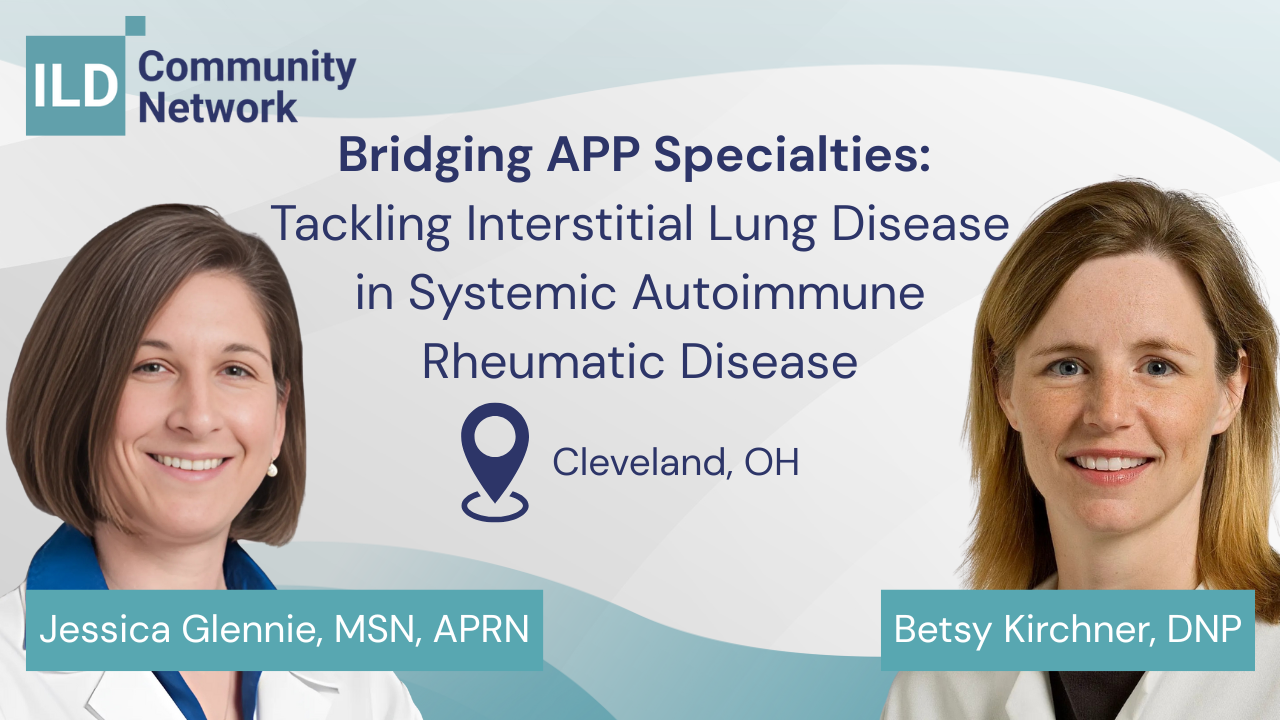
Bridging APP Specialties: Tackling Interstitial Lung Disease in Systemic Autoimmune Rheumatic Disease
 November 17 @ 06:30 pm - 09:00 pm EST
November 17 @ 06:30 pm - 09:00 pm EST
Register Today!..
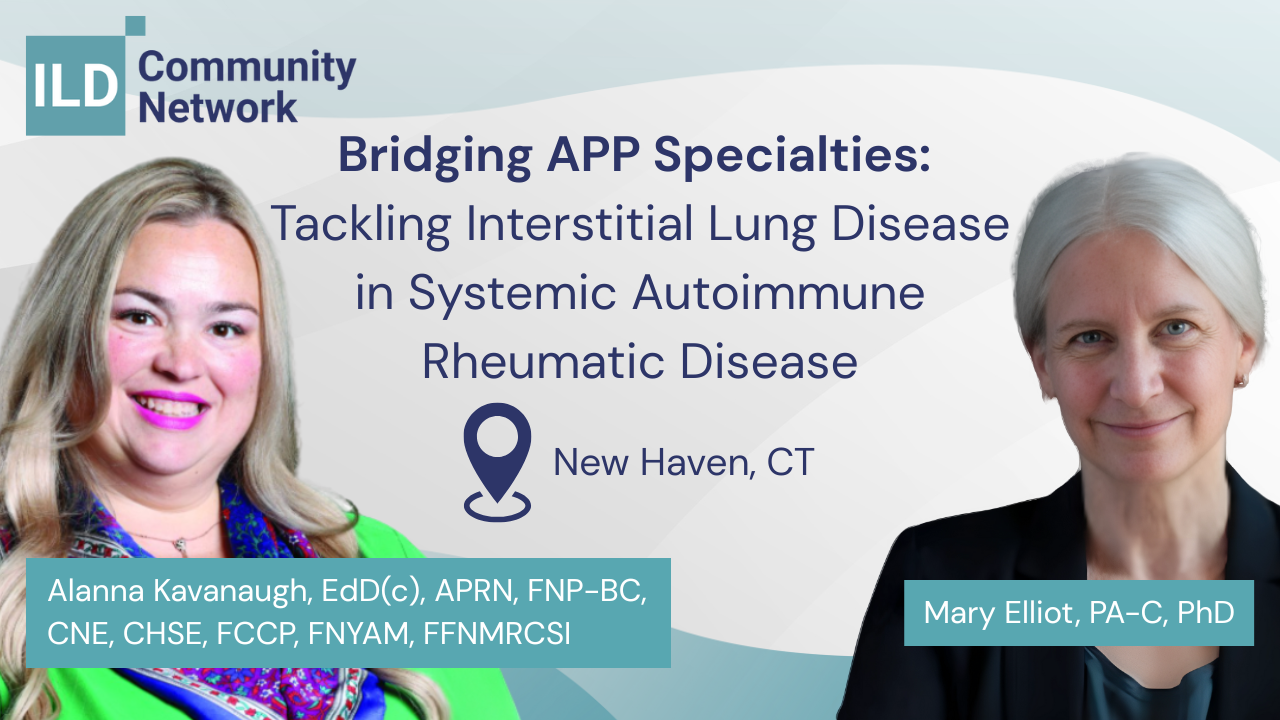
Bridging APP Specialties: Tackling Interstitial Lung Disease in Systemic Autoimmune Rheumatic Disease
 December 04 @ 06:30 pm - 09:00 pm EST
December 04 @ 06:30 pm - 09:00 pm EST
Register Today!..

CME EVENT
RhAPP Regional Chapter Summit
 December 06 @ 09:00 am - 12:30 pm EDT
December 06 @ 09:00 am - 12:30 pm EDT
Registration Details Coming Soon!..

CME EVENT
RhAPP Regional Chapter Summit
 January 16 @ 05:00 pm - 08:00 pm PST
January 16 @ 05:00 pm - 08:00 pm PST
Details Coming Soon!..
Bridging APP Specialties: Tackling Interstitial Lung Disease in Systemic Autoimmune Rheumatic Disease
 January 22 @ 06:30 pm - 09:00 pm CST
January 22 @ 06:30 pm - 09:00 pm CST
Register Today!..
Bridging APP Specialties: Tackling Interstitial Lung Disease in Systemic Autoimmune Rheumatic Disease
 January 22 @ 06:30 pm - 09:00 pm CST
January 22 @ 06:30 pm - 09:00 pm CST
Register Today! ..
Bridging APP Specialties: Tackling Interstitial Lung Disease in Systemic Autoimmune Rheumatic Disease
 December 03 @ 06:30 pm - 09:00 pm EST
December 03 @ 06:30 pm - 09:00 pm EST
Register Today! ..
Bridging APP Specialties: Tackling Interstitial Lung Disease in Systemic Autoimmune Rheumatic Disease
 January 27 @ 06:30 pm - 09:00 pm CST
January 27 @ 06:30 pm - 09:00 pm CST
Register Today! ..
ILD Digital Learning Center
Podcasts
Podcasts

ILD & PH-ILD at the Rheum–Pulm Crossroads
 November 2025
November 2025
 22:52 m
22:52 m
Join host Amanda Mixon, President of RhAPP, for a special episode recorded live at the 6th Annual RhAPP Conference. In this conversation, Amanda is joined by Jessica Glennie, CNP, from the Cleveland Clinic, to explore the complex intersection of rheumatology and pulmonology, focusing on Interstitial Lung Disease (ILD) and Pulmonary Hypertension in ILD (PH-ILD). Together, they unpack how early recognition, multidisciplinary collaboration, and evidence-based management can improve outcomes for patients with connective tissue disease–related pulmonary complications. Tune in for expert insights, practical diagnostic tips, and highlights from one of the most engaging sessions of the RhAPP National Conference.


Evolving IPF Care: The Significance of Nerandomilast’s FDA Approval
 October 2025
October 2025
 25:20 m
25:20 m
In this special crossover episode, host Amanda Mixon, PA-C, President of RhAPP, sits down with Corinne Young, FNP-C, founder and President of the Association of Pulmonary Advanced Practice Providers (APAPP), to discuss one of the most exciting developments in interstitial lung disease: the FDA approval of nerandomilast for idiopathic pulmonary fibrosis (IPF). This breakthrough marks the first new IPF therapy in more than a decade and introduces a novel PDE4B mechanism of action designed to reduce fibrosis and improve lung function. Together, Amanda and Corrine unpack the clinical data behind nerandomilast, key findings from the FIBRONEER-IPF trial, and how its safety profile—particularly reduced GI side effects—may reshape treatment pathways and patient quality of life. The conversation also highlights the overlap between rheumatology and pulmonology in managing fibrotic lung diseases and the importance of interdisciplinary collaboration as additional indications for progressive pulmonary fibrosis (PPF) are anticipated. #Rheumatology #Pulmonology #InterstitialLungDisease #IPF #Nerandomilast #Fibrosis #AdvancedPracticeProviders #APPs #FDAApproval #ClinicalUpdates


Rheumatology in the Lungs
 July 2025
July 2025
 24:47 m
24:47 m
How can Advanced Practice Providers (APPs) in rheumatology and pulmonology collaborate more effectively to manage interstitial lung disease (ILD) and connective tissue diseases (CTDs)? In this engaging episode of the APAPP Broadcast, recorded live at the Second Annual National APAPP Conference in Nashville, experts Jessica Glennie, PA-C (Cleveland Clinic), Amanda Mixon, PA-C (Colorado), and Cori Fratelli, NP (National Jewish Health) explore clinical overlaps between autoimmune rheumatic diseases and lung involvement, such as ILD in rheumatoid arthritis, systemic sclerosis (scleroderma), Sjögren’s syndrome, and myositis. The panel shares clinical pearls on: -How to recognize signs of CTDs in pulmonary patients -The importance of labs and imaging in early diagnosis -What rheumatology APPs should ask about pulmonary symptoms -The power of cross-specialty collaboration -Real-world case insights, including navigating bird-related hypersensitivity pneumonitis


Immunology of the Lung Podcast
 July 2025
July 2025
 11:40 m
11:40 m
Tune in from the Annual APAPP National Conference for a dynamic episode of the APAPP Podcast featuring Corinne Young, FNP-C, Amanda Michaud, PA-C, and Brian Bizik, PA-C—three expert APPs leading engaging sessions on lung immunology, rare immune deficiencies, and COPD updates. Amanda breaks down the “Immunology of the Lung 101” and her “Finding the Zebras” series, where she highlights key red flags for primary immune deficiencies, sharing real patient cases and diagnostic tips to help clinicians recognize and manage these commonly missed conditions. Brian shares practical takeaways from the latest GOLD COPD guidelines, including how biomarkers like eosinophil counts can guide personalized inhaled corticosteroid decisions. Whether you're managing patients with asthma, COPD, or unexplained recurrent infections, this episode delivers clinical pearls you can apply in your practice right away. Discover why this APP-led meeting stands out as a must-attend event for pulmonary and immunology providers. Be sure to like, subscribe, and follow us for more expert-driven conversations.


ILD 101, ILD 102, ILD Peds
 July 2025
July 2025
 20:57 m
20:57 m
Join Jessica Glennie, APRN, Naomi Miyazawa, PA-C, and Cori Fratelli, FNP, from the 2025 APAPP National Conference as they explore pediatric and adult interstitial lung disease (ILD). This episode covers diagnosis, disease progression, anti-inflammatory and anti-fibrotic therapies, and the importance of multidisciplinary care. Learn about pediatric ILD (CHILD), autoimmune-related ILD, and new treatment guidelines—all through real-world clinical insights.

Advancing ILD & PH-ILD Care
 July 2025
July 2025
 21:35 m
21:35 m
Join Jessica Glennie, APRN, and Lori Reed, FNP, from the 2025 APAPP National Conference as they discuss key insights in diagnosing and managing interstitial lung disease (ILD) and pulmonary hypertension (PH). From interpreting PFTs and recognizing red flags to exploring current and emerging therapies like inhaled treprostinil and neuredomast, this episode offers practical strategies for improving patient care. Tune in for expert tips and updates every pulmonary provider should know.

Practical Considerations for Screening for PH in ILD Clinics
 July 2025
July 2025
 17:17 m
17:17 m
In this insightful Podcast, expert advanced practice providers, Corinne Young & Jessica Glennie share practical strategies for identifying and screening for pulmonary hypertension (PH) in patients with interstitial lung disease (ILD). They discuss how to recognize subtle red flags—such as declining DLCO, changes in walk test performance, and discrepancies in pulmonary function test results—that may indicate the presence of PH. The conversation also covers when to order echocardiograms, when to refer for right heart catheterization, and how to distinguish ILD progression from the development of PH. With a focus on multidisciplinary collaboration and real-world clinical workflows, this episode offers valuable, actionable guidance for APPs, pulmonologists, and care teams managing ILD populations.


Understanding MAC with Jennifer Faber- Gerling
 December 2024
December 2024
 30:30 m
30:30 m
In this episode, Corinne Young interviews Jennifer Faber- Gerling about mycobacterium avian complex (MAC). They discuss the bacterium itself, the rise in cases, screening and diagnosis, treatment and side effects, reinfection versus reactivation, and symptom management. Jennifer emphasized the importance of close surveillance, collaboration with a multidisciplinary team, and individualized care for patients with MAC.


Idiopathic Shortness of Breath part 2 Dysfunctional Breathing Clinic
 December 2024
December 2024
 29:41 m
29:41 m
Nurse practitioner Cori Fratelli from National Jewish Health discusses breathing pattern disorders, related to unexplained dyspnea. Cori advocates to consider these disorders, discusses treatment methods like breath retraining, inspiratory muscle training, and emphasizes the need for more research and specialized clinics.
FAQ
FAQ


What Were The Key Findings From the FIBRONEER-IPF Study?
 October 2025
October 2025
 03:51 m
03:51 m
In this FAQ video, Corinne Young, FNP-C, founder and president of the Association of Pulmonary Advanced Practice Providers (APAPP), breaks down the pivotal FIBRONEER-IPF Phase 3 trial evaluating nerandomilast, a novel oral PDE4B inhibitor for patients with idiopathic pulmonary fibrosis (IPF). This randomized, double-blind, placebo-controlled study assessed nerandomilast both as monotherapy and in combination with existing antifibrotic therapies such as pirfenidone and nintedanib. Over 52 weeks, investigators observed that nerandomilast slowed lung function decline (FVC), reduced exacerbations and hospitalizations, and demonstrated a safety profile comparable to placebo, with notably fewer gastrointestinal side effects than traditional antifibrotics. These findings mark an exciting advancement in IPF management, offering clinicians a new therapeutic option that may improve both tolerance and long-term outcomes. #IPF #Nerandomilast #FIBRONEERIPF #Pulmonology #AntifibroticTherapy #PDE4B #InterstitialLungDisease #AdvancedPracticeProviders #APPs #ClinicalTrials #FDAApproval
Webcast
Webcast


Emerging Therapies in ILD
 October 2025
October 2025
 07:37 m
07:37 m
In this presentation, Corinne Young reviews the latest advances in therapies for interstitial lung disease (ILD) and idiopathic pulmonary fibrosis (IPF), highlighting the promising results of nerandomilast, a phosphodiesterase-4B inhibitor with both antifibrotic and immunomodulatory effects. Phase 3 trials (FIBRONEER-IPF and FIBRONEER-ILD) demonstrated that twice-daily nerandomilast slowed lung function decline and improved outcomes across patient populations, including those with autoimmune-related disease. The discussion also covers the drug’s safety profile—showing fewer gastrointestinal side effects compared to existing antifibrotic agents—and emerging treatments such as inhaled treprostinil, which is being studied for pulmonary fibrosis beyond pulmonary hypertension. With multiple new agents and combination therapies on the horizon, these developments represent meaningful progress in the treatment and management of fibrotic lung disease.


Antifibrotic Therapy
 October 2025
October 2025
 06:40 m
06:40 m
In this session, Corinne Young reviews the evolution of antifibrotic therapies for interstitial lung disease, beginning with the 2015 U.S. approval of pirfenidone (Esbriet) for idiopathic pulmonary fibrosis (IPF). Pirfenidone works by targeting TGF-β and TNF-α to slow fibroblast proliferation and collagen synthesis, though patients often experience gastrointestinal side effects and fatigue. The discussion also covers nintedanib (Ofev), a tyrosine kinase inhibitor that blocks multiple growth factor pathways (VEGF, FGF, PDGF) and is now approved for both IPF and other progressive fibrotic lung diseases. Clinical trials such as CAPACITY, ASCEND, INPULSIS, and INBUILD demonstrated that these antifibrotics significantly slow the rate of lung function decline and disease progression. The talk concludes by emphasizing careful side-effect management, liver monitoring, and appropriate patient selection to optimize outcomes with these cornerstone antifibrotic therapies.

The Rheum-Pulm Interface: Bridging Specialties in SARD-ILD
 October 2025
October 2025
 11:21 m
11:21 m
In this session, Corinne Young and Wendy Simmons highlight the importance of a multidisciplinary approach to managing interstitial lung disease (ILD) in patients with systemic autoimmune and rheumatologic disorders. Collaboration between rheumatology, pulmonology, and radiology teams is key to early recognition, diagnosis, and treatment planning—especially given the high risk of ILD-related morbidity and mortality in conditions like systemic sclerosis, rheumatoid arthritis, lupus, and Sjögren’s syndrome. The discussion reviews ACR screening guidelines, emphasizing the role of high-resolution CT imaging, pulmonary function testing, and oxygen desaturation monitoring. It also covers evidence-based first-line and escalation therapies, including mycophenolate, cyclophosphamide, and rituximab, while underscoring the need for frequent assessment, early intervention, and coordinated care to improve patient outcomes.

Understanding the Landscape of ILD: Burden, Pathophysiology, and Classification
 October 2025
October 2025
 20:49 m
20:49 m
In this presentation, pulmonary nurse practitioner Corinne Young and rheumatology physician assistant Wendy Simmons explore the complex relationship between interstitial lung disease (ILD) and connective tissue diseases (CTDs). Together, they provide a multidisciplinary perspective—highlighting how collaboration between pulmonology, rheumatology, and radiology leads to earlier diagnosis, better management, and improved outcomes. The session covers ILD classifications, common causes such as autoimmune disorders, environmental exposures, and drug toxicities, as well as diagnostic tools including high-resolution CT imaging, pulmonary function testing, and serologic assays. The speakers also discuss the importance of recognizing progressive phenotypes, understanding imaging patterns like UIP and NSIP, and tailoring therapy based on disease behavior. This session emphasizes that in ILD, time is lung—early recognition and coordinated care are essential to preserving function and extending quality of life.

IPF & PPF: Natural History, Diagnosis, and Management
 October 2025
October 2025
 07:52 m
07:52 m
In this educational session, Corinne Young breaks down the underlying mechanisms, progression, and management of idiopathic pulmonary fibrosis (IPF) and other interstitial lung diseases (ILDs). The discussion covers common genetic and environmental risk factors—including family history, smoking, and occupational exposures—and explains how chronic inflammation leads to fibrosis and loss of lung elasticity. Listeners gain a clear understanding of how progressive pulmonary fibrosis is identified through lung function tests (FVC, DLCO) and imaging changes over time. The presentation also addresses treatment strategies, highlighting when corticosteroids may be appropriate, why long-term steroid use is limited, and how newer antifibrotic and immunomodulatory therapies are improving outcomes for patients with fibrotic lung disease.

Rheumatoid Arthritis Associated ILD, End Stage Therapy, and Multidisciplinary Care
 October 2025
October 2025
 02:31 m
02:31 m
In this discussion, Corinne Young explores the complexities of managing patients with advanced interstitial lung disease, emphasizing the importance of early referral for lung transplant and cautious evaluation of unproven stem cell therapies. The conversation highlights how patients are sometimes misled into costly, non-evidence-based treatments abroad and underscores that only limited data exist for hematopoietic stem cell use in this setting. The speakers stress the critical role of multidisciplinary collaboration among pulmonology, rheumatology, gastroenterology, and cardiology teams, along with early conversations about palliative care and quality-of-life goals. With new therapies emerging, the focus remains on preserving lung function, aligning treatment with patient priorities, and ensuring compassionate, coordinated care for those facing progressive disease.

What Can Pulmonology APPs Do Once They've Established an ILD Diagnosis to Aid in Potential Rheumatology Workups?
 July 2025
July 2025
 01:42 m
01:42 m
Once you've confirmed a diagnosis of interstitial lung disease (ILD), what’s next? In this practical and fast-paced discussion, Amanda Mixon, PA-C, shares actionable steps for evaluating patients for underlying autoimmune or connective tissue diseases. Learn what symptoms to ask about—joint pain, morning stiffness, skin lesions, Raynaud’s, dry eyes or mouth—and how labs and rheumatology collaboration can support early detection and accurate diagnosis. This video offers clinical pearls for APPs working in pulmonology who want to strengthen their diagnostic acumen and build better cross-specialty communication with rheumatology colleagues. Topics covered: – What symptoms may signal underlying rheumatic disease in ILD patients – Key lab tests to guide your differential – When to refer to rheumatology – The value of real-time collaboration across specialties ILD care is better together. Watch now to improve your approach to autoimmune workups in pulmonary patients.


Scleroderma Treatment
 July 2025
July 2025
 01:52 m
01:52 m
In this focused discussion, Amanda Mixon, PA-C shares a practical approach to managing patients with systemic sclerosis (Scleroderma), with an emphasis on individualized care based on disease manifestation. From echocardiograms to pulmonary imaging, medication choices to vascular complications, this talk provides key insights into how APPs can tailor care to improve outcomes. Learn how to approach limited vs. diffuse Scleroderma, when to avoid glucocorticoids, and how to manage complications like digital ulcers and pulmonary involvement. Key takeaways include: – When to use echocardiograms, CT scans, and other diagnostics – Medication strategies: Mycophenolate, Selenomab, CCBs, ARBs, and more – Avoiding glucocorticoids in diffuse disease and managing risk of renal crisis – Treating symptomatically: digital ulcers, skin fibrosis, and blood flow support This is a must-watch for APPs in rheumatology, pulmonology, or primary care managing patients with Scleroderma.

Systemic Sclerosis Presentation
 July 2025
July 2025
 11:52 m
11:52 m
In this powerful and personal clinical reflection, Amanda Mixon, PA-C, shares her journey treating patients with diffuse systemic sclerosis (Scleroderma), including key lessons learned from working at a major Scleroderma center at Northwestern. From building trust with colleagues to managing life-threatening complications like Scleroderma Renal Crisis, this video offers invaluable insights for APPs and clinicians navigating this complex autoimmune disease. You’ll hear firsthand experiences treating patients with severe skin involvement, pulmonary fibrosis, digital ulcers, GI complications, and early vasculopathy. Learn why RNA polymerase III positivity is a red flag, how to differentiate diffuse from limited SSc, and why early diagnosis and treatment are essential. What you’ll learn: – What distinguishes diffuse Scleroderma from limited forms – Clinical signs to recognize early: Raynaud’s, skin tightening, telangiectasia – The dangers of steroid use and Scleroderma Renal Crisis – Why collaboration and early referral to SSc centers can save lives – Real stories and clinical pearls from treating high-risk patients This is a must-watch for any clinician managing autoimmune diseases—especially those treating interstitial lung disease, GI complications, or vasculitis related to Scleroderma.

Idiopathic Inflammatory Myopathies and Pulmonary Disorders Including ILD
 July 2025
July 2025
 04:59 m
04:59 m
Inflammatory myopathies—like dermatomyositis, polymyositis, and inclusion body myositis—can be difficult to diagnose and manage, especially when they overlap with interstitial lung disease (ILD). In this clinical discussion, Amanda Mixon, PA-C, breaks down what to look for, from subtle signs like "mechanic's hands" to more serious red flags like MDA5-positive rapidly progressive ILD. Special attention is given to anti-synthetase syndrome, a condition often associated with ILD, arthritis, and elevated CK levels, and how antibody testing (e.g., Jo-1, SSA, MDA5) can guide diagnosis and urgency of care. You’ll also learn how to approach cancer screenings in patients with dermatomyositis and why a full malignancy workup is essential. What you'll learn: – How to identify anti-synthetase syndrome and inflammatory myopathies – Key clinical signs: weakness, mechanic’s hands, non-erosive arthritis – Understanding the myositis antibody panel and its clinical utility – The connection between dermatomyositis and malignancy risk – When and how to conduct a thorough cancer screening – Treatments including JAK inhibitors, IVIG, and rituximab Perfect for APPs, pulmonologists, and rheumatology teams, this video empowers you to catch early signs, personalize diagnostics, and take action.

Limited Cutaneous Scleroderma Presentation
 July 2025
July 2025
 01:48 m
01:48 m
In this quick but focused clinical overview, Amanda Mixon, PA-C, explains how to identify and differentiate limited systemic sclerosis (also known as CREST syndrome) from diffuse scleroderma. Associated with centromere antibodies, limited scleroderma primarily affects the distal extremities and face, and while skin involvement is less severe, patients face distinct long-term risks—especially pulmonary hypertension. This video breaks down the classic CREST acronym (Calcinosis, Raynaud’s, Esophageal dysmotility, Sclerodactyly, and Telangiectasias), along with practical tips for early recognition and long-term management. What you'll learn: – How to recognize clinical features of limited scleroderma – The role of centromere antibodies vs. SCL-70 in diagnosis – Early signs like Raynaud’s and esophageal symptoms – What to monitor for in years 5–10: pulmonary hypertension, vascular disease – Differentiating CREST from diffuse disease This is an essential update for APPs and clinicians managing autoimmune connective tissue disease, especially in patients with progressive symptoms involving the skin, GI tract, and lungs.


Sjogren’s Disease and ILD
 July 2025
July 2025
 01:43 m
01:43 m
In this concise and clinically insightful discussion, Amanda Mixon, PA-C, breaks down what to look for when suspecting Sjögren’s syndrome—an autoimmune condition marked by chronic dry eye and dry mouth, fatigue, and systemic manifestations. Often associated with SSA and SSB antibodies, Sjögren’s can overlap with interstitial lung disease (ILD), making it especially important for pulmonary and rheumatology providers to recognize early. Learn how to distinguish classic symptoms from environmental causes, when to consider antibody testing, and which patients may be at higher risk for more severe complications like ILD. What you’ll learn: – Clinical clues for identifying Sjögren’s in practice – Role of SSA and SSB antibodies in diagnosis – Recognizing extra-glandular manifestations: fatigue, arthritis, rashes – When to suspect ILD in Sjögren’s patients – Medication options and early steroid use considerations Whether you’re in primary care, pulmonology, or rheumatology, this video equips you to ask the right questions and understand the systemic risks behind what may appear to be “just dry mouth.”
Industry Resources
Identifying and Monitoring Autoimmune ILD | Insights in ILD
Pulmonary Function Tests (PFTs) Pocket Guide | Insights in ILD
HRCT Pocket Guide | Insights in ILD
History Taking Pocket Guide | Insights in ILD

WANT EXPERT PERSPECTIVES ON INTERSTITIAL LUNG DISEASE?
Imaging Atlas of Interstitial Lung Diseases | Insights in ILD
Rad Rounds UIP to IPF Mobile Application
Rad Rounds - UIP to IPF is an innovative, peer-reviewed resource that provides practicing and future pulmonologists and radiologists with training and references for recognizing and evaluating usual interstitial pneumonia (UIP) and interstitial lung diseases (ILDs) on high resolution computed tomography (HRCT). Through this application the user can access learning materials such as a step-by-step pattern recognition algorithm, utilizing user-provided HRCT scans, an interactive UIP/ILD glossary and image gallery to further assist in the evaluative process, several “test your knowledge” quizzes, and a series of short informational videos, covering subjects such as: Basic HRCT Technique, Imaging Positions, and Recognizing Features of ILD on HRCT. This app is ideal for: radiologists that would like to use the interactive algorithm to help assess their HRCT scans, pulmonologists that want to evaluate their own cases or learn more about HRCT in the diagnosis of ILD, and medical students and residents that want to learn about HRCT and ILD. Download now and find out: Is It UIP? Available on the App Store: https://apps.apple.com/us/app/rad-rounds-uip-to-ipf/id1327938328 Available on Google Play: https://play.google.com/store/apps/details?id=com.boehringer.radiologyrounds&hl=en_US
News
News

Aetiologic diagnosis of thoracic granulomatous diseases: a retrospective multicentre study in South-Central China
 November 2025
November 2025
CONCLUSIONS: Most thoracic granulomas arise from mycobacterial or fungal infection, while sarcoidosis is the leading non-infectious cause. Thoracoscopy and surgical biopsy show superior diagnostic yields, and special staining aids differentiation of fungal aetiologies. Findings support a multidisciplinary approach to improve diagnostic accuracy.

Characterisation of patients with antifibrotic-treated non-idiopathic pulmonary fibrosis progressive pulmonary fibrosis: a retrospective real-life study
 November 2025
November 2025
CONCLUSIONS: In our cohort, the underlying diagnoses and immunomodulatory treatments received significantly differed from those in the phase III licensing trial. More patients received nintedanib at a reduced dose than at a full dose, despite limited evidence of its efficacy and effectiveness. This highlights the large gap in evidence and the need for additional real-world data.

Detection of Anti-MDA5 Autoantibodies Using HeLa Cells and Immunocytochemistry with Light Microscopy
 November 2025
November 2025
Anti-MDA5 autoantibodies are critical biomarkers for dermatomyositis (DM), amyopathic dermatomyositis (CADM), and polymyositis (PM), particularly in identifying patients at risk of rapidly progressive interstitial lung disease (RP-ILD). Early detection of these autoantibodies is essential to improve patient outcomes, as delayed diagnosis often leads to poor prognoses. Currently, radioimmunoassay is the gold standard for detecting anti-MDA5, but its use is limited by high costs, lengthy...

ML385 Attenuates Malignant Progression of Silica-induced Lung Adenocarcinoma Cells through the ROS/NRF2-autophagy Axis Pathway
 November 2025
November 2025
Silica exposure is associated with an increased risk of lung adenocarcinoma, but its molecular mechanism remains unclear. This study aims to establish a repeatable experimental protocol to explore how the nuclear factor erythroid 2-related factor 2 (NRF2) inhibitor ML385 inhibits silica-induced malignant progression of lung adenocarcinoma by regulating the ROS/NRF2-autophagy axis pathway. Firstly, a silicosis model was established by intranasal perfusion of silica suspension in C57BL/6 mice. The...

The Italian Society for Rheumatology guidelines for the treatment of patients with rheumatoid arthritis and interstitial lung disease
 November 2025
November 2025
CONCLUSIONS: These guidelines represent a fundamental step towards improving the health management of patients with rheumatological diseases in Italy by providing specific and evidence-based guidelines for the management of RA-ILD. Their use is intended to promote health and reduce the burden of morbidity and mortality in this vulnerable population.

Serum carcinoembryonic antigen levels correlate with disease severity and one-year survival across different interstitial lung diseases subtypes
 November 2025
November 2025
CONCLUSIONS: Serum CEA levels are associated with disease severity and 1-year mortality across ILD subtypes, supporting its potential as a reliable prognostic biomarker.

Efficacy and safety of ARX788 for individuals with HER2-positive breast cancer and brain metastases (ACE-Breast-06): a single-arm, phase 2 trial in China
 November 2025
November 2025
BACKGROUND: ARX788 is a next-generation antibody-drug conjugate (ADC) in which an anti-HER2 monoclonal antibody is linked to a monomethyl auristatin F (MMAF) payload. This study aimed to investigate the intracranial efficiency of ARX788 in epidermal growth factor receptor 2 (HER2)-positive breast cancer with active brain metastases.

Editorial: Pulmonary involvement in systemic autoimmune rheumatic diseases (SARDs): from diagnostic tools to therapeutic strategies
 November 2025
November 2025
No abstract

Interstitial lung disease following combined CDK4/6 inhibitor therapy and radiotherapy in advanced breast cancer: a case report
 November 2025
November 2025
CONCLUSION: These cases suggest that CDK4/6i may potentiate radiotherapy-associated pulmonary toxicity, and clinicians should exercise caution with this combination.

Cytokine Expression Profiling in Idiopathic Pulmonary Fibrosis: Insights From Integrative Proteomic Analysis
 November 2025
November 2025
CONCLUSIONS: Using protein microarrays, we obtained comprehensive cytokine expression profiles in control and IPF lung tissues and conducted an integrated bioinformatics analysis of the proteomic data. Our findings may improve the comprehension of the role of cytokines in IPF and the underlying mechanisms. Moreover, they provide novel targets for developing safe and efficacious drugs for treating IPF.

Pathogenic expansion: fibroblast proliferation fuels fibrosis
 November 2025
November 2025
Pulmonary fibrosis, an unrelenting disease of lung scarring, has been associated with the expansion of a profibrotic fibroblast population and extensive extracellular matrix deposition. In this issue, Molina and colleagues provide foundational mechanistic evidence that fibroblast proliferation itself is a critical driver of fibrosis. Using lineage tracing in preclinical fibrosis models, the authors showed that naive Scube2+ alveolar fibroblasts underwent a profibrotic phenotypic switch prior to...

Phenotypic Analysis of Pulmonary Hypertension Associated With Low Diffusion Capacity and Preserved Lung Function
 November 2025
November 2025
Severe diffusion impairment in pulmonary arterial hypertension (PAH), particularly in idiopathic PAH (IPAH), has garnered considerable attention. However, comprehensive data on low diffusion capacity of the lungs for carbon monoxide (DLCO) with preserved lung function remain limited in broader pulmonary hypertension (PH) cohorts. We analyzed patients with PH, preserved lung function, low DLCO, and available computed tomography (CT) scans. The analysis included 117 patients, with 34% cases of...

When scars tell a story: cases of scar sarcoidosis preceding or following diagnosis of systemic disease
 November 2025
November 2025
Sarcoidosis is a systemic granulomatous disease of unknown etiology, characterized by the formation of non-necrotizing granulomas in various organs, with the lungs and mediastinal lymph nodes being the most commonly affected sites. "Scar sarcoidosis" refers to the rare phenomenon in which sarcoid granulomas develop in pre-existing scars, such as surgical scars, tattoos, or sites of previous skin trauma. We report two cases of patients who presented with sarcoid granulomas developing in previous...

Performance of pulmonary physical exam skills by internal medicine interns
 November 2025
November 2025
CONCLUSIONS: Medicine interns had variable skills in performing the pulmonary PE. Improving PE skills would lead to increased identification of relevant pulmonary findings, inform clinical decision making, and improve overall patient care.

The thoracic radiographic unstructured interstitial pattern underestimates and may fail to identify canine respiratory disease compared to computed tomography
 November 2025
November 2025
In dogs, lung disease presenting with a radiographic unstructured interstitial pattern (UnIP) poses a diagnostic challenge due to heterogenous clinical signs, non-specific differentials, and need for tissue sampling to confirm the pathologic process. The terminology describing patterns on thoracic radiography (TR) can be misleading in assuming an interstitial pattern implies disease of the pulmonary interstitium. Thoracic computed tomography (CT) is more likely to predict anatomic localization...

Efficacy and safety of trastuzumab deruxtecan for metastatic HER2+ and HER2-low breast cancer: A systematic review and meta-analysis
 November 2025
November 2025
CONCLUSION: T-DXd has significant long-term and near-term efficacy in prolonging median overall survival, median PFS, and increasing the objective remission rate in patients with HER2-positive or low-expression breast cancer; however, the treatment is associated with notable adverse events, and physicians should be alert to the occurrence of serious adverse events when using this drug.

An AMPK-Centric Strategy: Foenumoside B Coordinates PINK1/Parkin-Mediated Mitophagy With Nrf2/HO-1 Antioxidant Signaling to Resolve Oxidative Stress in Radiation-Induced Lung Injury
 November 2025
November 2025
Radiation-induced lung injury (RILI) is a dose-limiting toxicity of thoracic radiotherapy driven by mitochondrial damage-mediated oxidative stress, persistent DNA damage, and senescence, which together destabilize the alveolar-interstitial niche and promote fibrosis. Here, we identify Foenumoside B (FSB), a natural saponin from Lysimachia foenum-graecum, as a dual-action modulator that preserves mitochondrial quality and restores systemic redox homeostasis to attenuate RILI. In a murine total...

Genetic causal association between metabolic syndrome and idiopathic pulmonary fibrosis: A 2-sample Mendelian randomization
 November 2025
November 2025
Prior epidemiological investigations have indicated a linkage between metabolic syndrome (MetS) and idiopathic pulmonary fibrosis (IPF). The objective of the present research was to elucidate the inherited causal relationship of MetS with IPF. A 2-sample Mendelian randomization (MR) design was adopted to assess the genetic cause-effect link between MetS and IPF. Multiple analytical strategies, such as inverse-variance weighted (IVW), MR-Egger, weighted median, and weighted mode, were...

Differentiating respiratory syncytial virus pneumonia from interstitial lung disease associated with systemic sclerosis: A case report
 November 2025
November 2025
RATIONALE: Respiratory syncytial virus (RSV) is a common cause of lower respiratory tract infections in older adults. In systemic sclerosis, interstitial lung disease is a frequent, serious complication requiring immunosuppressive therapy. Differentiating RSV pneumonia from systemic sclerosis-associated interstitial lung disease (SSc-ILD) is essential for appropriate management and to avoid initiating immunosuppressive agents that may be harmful in cases of RSV pneumonia.

Pilot study of (18)F-FAPI-RGD PET/CT for the diagnosis of connective tissue disease associated interstitial lung disease
 November 2025
November 2025
No abstract
Testimonials
"The ILD Alliance of RhAPP & APAPP will provide our growing APP community with valuable resources to better educate and connect with ILD Experts based on your region."
"The ILD Alliance of RhAPP & APAPP will provide our growing APP community with valuable resources to better educate and connect with ILD Experts based on your region."
Amanda Mixon

"At the end of the day, it is all about our patients. Having a place where we can interact and learn from other ILD Experts in our community will only make our day-to-day patient care stronger and more effective."
"At the end of the day, it is all about our patients. Having a place where we can interact and learn from other ILD Experts in our community will only make our day-to-day patient care stronger and more effective."
Jessica Glennie

"Thanks to the ILD Alliance, I was able to connect with another APP in my region to discuss a few questions I had."
"Thanks to the ILD Alliance, I was able to connect with another APP in my region to discuss a few questions I had."
Daric Mueller

"I listened to the "Deep Dive Into ILD Therapeutics" podcast with Jessica Glennie and Cori Fratelli on my way to work. Podcasts like these help us understand what options we have to best treat our patients."
"I listened to the "Deep Dive Into ILD Therapeutics" podcast with Jessica Glennie and Cori Fratelli on my way to work. Podcasts like these help us understand what options we have to best treat our patients."
Felicia Mackey

"Being able to connect with other APPs in your region who are in different specialties is invaluable! I hope there are more alliances like these in the future."
"Being able to connect with other APPs in your region who are in different specialties is invaluable! I hope there are more alliances like these in the future."
Jeannette Hart






